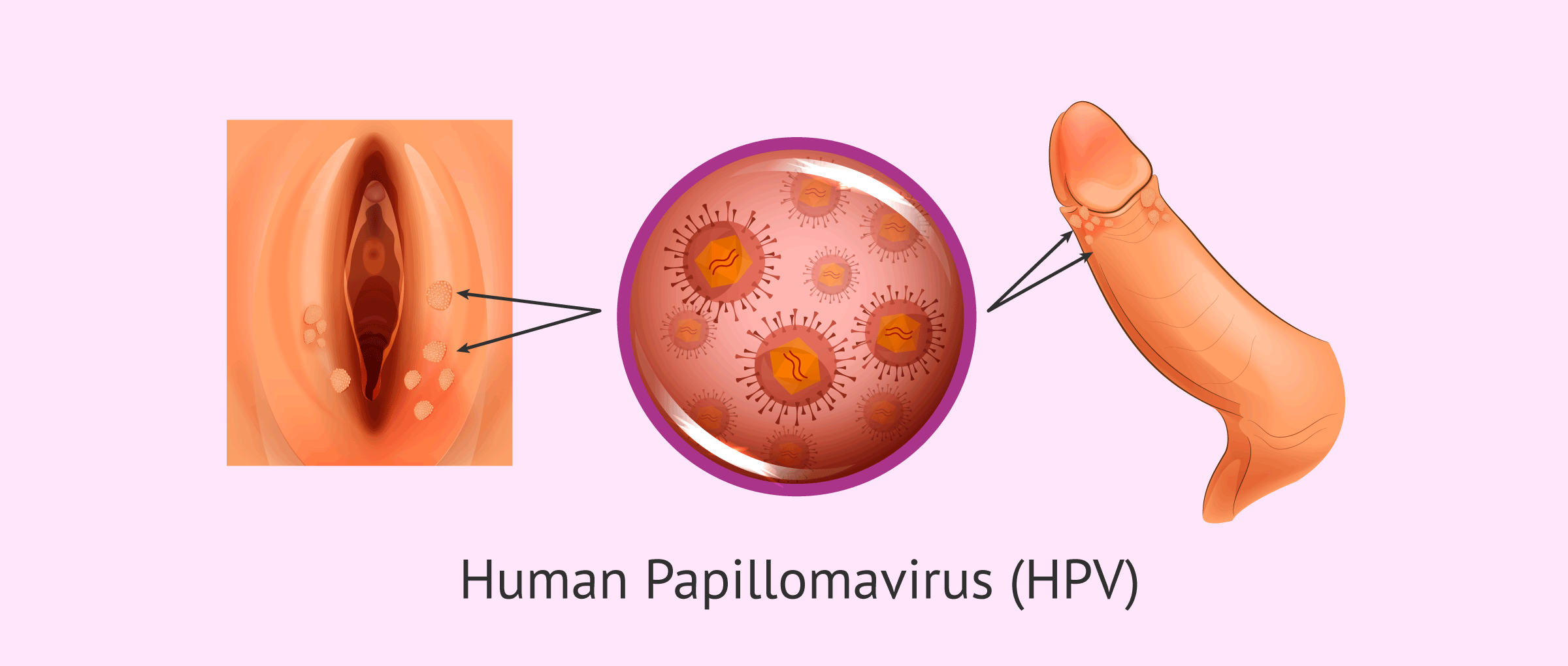
Human papillomavirus (HPV) is a sexually transmitted infection that is transmitted by direct contact during sexual intercourse.
Sometimes HPV is asymptomatic and goes unnoticed, but it can have serious long-term consequences, such as cervical cancer.
In this article we are going to detail the different types of papillomavirus, how it is transmitted and the forms of prevention and treatment.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
- 8.
Human papillomavirus
HPV is the most common sexually transmitted disease (STD). About 75% of the sexually active population will become infected with HPV at some point in their lives, especially between the ages of 15 and 25.
The vast majority of HPV infections are harmless and go away spontaneously. However, some types of HPV can cause genital warts or cancer.
In women, papillomavirus infection is the leading cause of cervical cancer, so annual gynecological checkups are important.
Types
There are more than 200 related types of papillomavirus, but only about 40 of them are sexually transmitted by bringing the skin and mucous membranes of the vulva, vagina, cervix, rectum, anus, penis, and scrotum into direct contact, as well as the mouth and throat.
Human papillomavirus types are classified as follows:
- Low risk
- are the ones that cause genital warts (condylomata acuminata). In 90% of cases, these are HPV types 6 and 11.
- High risk
- are those related to cancer of the cervix, although to a lesser extent they can also lead to cancer of the vulva, vagina, penis, anus, mouth and throat. There are about 12 high-risk types of HPV, but the most common are types 16 and 18.
How does infection occur?
As we have said, the human papillomavirus is spread through unprotected sex.
To be more specific, HPV infection can occur both vaginally and anal, when there is direct contact between the skin or mucous membranes of an infected person and a healthy person.
It should also be noted that HPV can be transmitted through oral sex. In fact, in recent years there has been an increase in cases of throat and mouth cancer caused by the human papillomavirus.
A person can become infected with HPV even without ejaculation or penetration. The simple direct contact between the vulva, vagina, penis, anus, and mouth is enough for the human papillomavirus to spread.
Symptoms and Consequences
Most HPV infections in young women are temporary and unimportant, disappearing after one or two years.
In most cases, HPV has no serious symptoms or pathologies, while in other cases genital warts or condylomata appear. These are fleshy, soft protuberances that resemble a miniature cauliflower.
These warts are painless and, like any other type of wart, can be easily removed by burning them with nitrogen.
In infections of the most serious types of HPV, on the other hand, the person may develop the following types of cancer:
- Cervical Cancer
- Anal Cancer
- Oropharyngeal Cancers
- Vaginal Cancer
- Vulva Cancer
- Penile Cancer
Almost all cases of cervical cancer are caused by the human papillomavirus. Unfortunately, the signs and symptoms of this type of infection may not manifest until it is in an advanced stage.
The development of uterine cancer is slow. First there are precancerous lesions that can eventually progress to invasive cervical cancer over the course of about 15-20 years.
This offers many opportunities for detection and treatment of precancerous lesions, often with high cure rates. You can get more detailed information on this topic in the following article:
Prevention and Diagnosis
Because most women infected with HPV do not know they are infected or do not have symptoms, it is very important to have a Pap smear every year to detect abnormal changes in the cells of the cervix.
There is also a more specific test that can detect some high-risk virus types: the HPV screening test.
Since these HPV screening and early diagnosis tools were developed, deaths from cervical cancer have decreased significantly over the past 50 years.
Specialists advise to start gynecological check-ups every year from the moment the woman begins to have sex.
The use of barrier contraceptive methods for vaginal, anal, or oral sex is essential to reduce the risk of human papillomavirus transmission, even when the person has no symptoms.
HPV Vaccines
Currently, there are three vaccines aimed at the prevention of human papillomavirus: Cervarix®, Gardasil® and Gardasil®9.
They all prevent infection with HPV types 16 and 18, which cause 70% of cervical cancer cases.
Everyone between the ages of 9 and 45 can be vaccinated against HPV, with the following considerations in mind:
- People ages 9 to 14 need only two shots of the vaccine, given 6 months apart.
- People between the ages of 15 and 45 need three shots of the vaccine. The second dose is administered after 2 months of the first and the third after 4 months of the second.
- It is best for all boys and girls ages 11-12 to be vaccinated to be protected from HPV before they begin their sex lifes.
- It is not common to get an HPV vaccine after age 26.
- The vaccine does not treat an HPV infection, but it does work to protect against other types of the virus.
It is best to consult your doctor if it is advisable to be vaccinated against HPV, regardless of the person's sex and age.
Cervarix®
The Cervarix® vaccine contains as active ingredients the protein L1 of human papillomavirus types 16 and 18.
As mentioned above, these are the types of HPV that are most likely to cause cervical cancer.
Gardasil®
In addition to protecting against infection with HPV types 16 and 18, Gardasil® also offers protection against serotypes 6 and 11, which cause 90% of genital warts.
On the other hand, the Gardasil®9 vaccine also protects against five other types of HPV: 31, 33, 45, 52 and 58. With this vaccine, protection against precancerous HPV lesions is greater than 90%.
Finally, it should be noted that while the administration of these vaccines is very relevant, they do not protect women from all types of HPV that cause cervical cancer, so the Pap smear should continue to be performed periodically even after the vaccine has been received.
FAQs from users
Are fertility treatments possible in women infected with HPV?
Yes, HPV is not a contraindication for pregnancy or assisted reproductive techniques, as long as the virus has not caused any injury to the cervix, vagina or external genitalia. For this reason, all women undergoing treatment will be asked for a Pap smear beforehand. If any lesion is present, we will have to wait for it to resolve, but if the HPV is present and the Pap is negative and there are no lesions, we will be able to go ahead with the process without any problem. The woman will just have to follow her usual check-ups.
Can human papillomavirus be cured?
Currently, there is no cure for HPV, but there are ways to prevent it, such as vaccines for high-risk types of HPV and those that cause genital warts.
Normally, it is the body's immune system that is responsible for fighting HPV before it leads to more severe symptoms. For this purpose, the immune system makes antibodies directed at the HPV until it disappears.
Only precancerous lesions that may appear on the cervix, vagina, etc. as a result of high-risk HPV infection are treated.
Can the human papillomavirus be transmitted during breastfeeding?
Although it is true that human papillomavirus DNA has been found in breast milk samples, the risk of transmission to the baby during breastfeeding is practically non-existent.
Also, no cases of transmission to the baby have been found even when the mother had lesions on the nipple. HPV infections are therefore compatible with breastfeeding.
Suggested for you
If you want to continue reading about other types of sexually transmitted diseases, you can access the following post: STDs in men and women.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!



does hpv cause sterility
Hello,
When left untreated HPV, as many other STD’s, may lead to infertility. Normally, there shouldn’t be any problems in conceiving though.
Hope this helps
Best
Hey folks,
I had sexual intercourse recently despite having hpv. We used protection though.
Soo my question is would hpv be contagious in case no condom is being used? Is it also possible to transmit the virus orally?? or through any other means?
Hello sarabrown,
Infectious diseases such as HPV can spread in a variety of ways- through the air, from direct or indirect contact with another person as well as through
urine, blood, body secretions and sexual contact.
So in short, yes there’s risk of having transmitted HPV to your sexual partner.
Hope this helps,
Romina
does hpv infection kill you??
Hello Murrielle,
normally, when detected at an early stage, not. In case of HPV infection, make sure you consult your gynecologist for further proceedings, though.
Hope I could resolve your question.
Regards