The summer of 1952 was hot, even by Texas standards: 25 days above 100F (38C), the “cool” days not much cooler. But across the state, swimming pools were shut. Cinemas, too, and bars and bowling alleys. Church services were suspended. Cities doused their streets with DDT insecticide; by now, health officials knew that mosquitoes didn’t spread the disease, but they had to be seen to be doing something. Nothing seemed to work. As the summer wore on, the numbers of polio cases grew.
One day in July, in a quiet Dallas suburb, a six-year-old boy named Paul Alexander was playing outside in the summer rain. He didn’t feel well – his neck hurt, his head pounded. Leaving his muddy shoes in the yard, he walked barefoot into the kitchen, letting the screen door slam behind him. When his mother looked up at his feverish face, she gasped. She made him run out and grab his shoes, then ordered him to bed.
Paul spent the first day in his parents’ bed, filling in Roy Rogers colouring books. But even as his fever soared and aching pains blossomed in his limbs, the family doctor advised his parents not to take him to hospital. It was clear that he had polio, but there were just too many patients there, the doctor said. Paul had a better chance of recovering at home.
Over the next few days, the boy’s condition worsened. Five days after he had walked into the kitchen barefoot, Paul could no longer hold a crayon, speak, swallow or cough. His parents rushed him to Parkland hospital. Though the staff were well trained and there was a dedicated polio ward, the hospital was overwhelmed. There were sick children everywhere, and nowhere to treat them all. Paul’s mother held him in her arms and waited.
When the boy was finally seen by a doctor, his mother was told that there was nothing to be done for him. Paul was left on a gurney in a hallway, barely breathing. He would have died had another doctor not decided to examine him again. This second doctor picked him up, ran with him to the operating theatre and performed an emergency tracheotomy to suction out the congestion in his lungs that his paralysed body couldn’t shift.
Three days later, Paul woke up. His body was encased in a machine that wheezed and sighed. He couldn’t move. He couldn’t speak. He couldn’t cough. He couldn’t see through the fogged windows of the steam tent – a vinyl hood that kept the air around his head moist and the mucus in his lungs loose. He thought he was dead.
When the tent was eventually removed, all he could see were the heads of other children, their bodies encased in metal canisters, nurses in starched white uniforms and caps floating between them. “As far as you can see, rows and rows of iron lungs. Full of children,” he recalled recently.

The next 18 months were torture. Although he couldn’t talk because of the tracheotomy, he could hear the cries of other children in pain. He lay for hours in his own waste because he couldn’t tell the staff he needed to be cleaned. He nearly drowned in his own mucus. His parents visited almost every day, but his existence was unrelentingly boring. He and the other children tried to communicate, making faces at each other, but, Paul said: “Every time I’d make a friend, they’d die.”
Paul recovered from the initial infection, but polio left him almost completely paralysed from the neck down. What his diaphragm could no longer do for him, the iron lung did. Paul lay flat on his back, his head resting on a pillow and his body encased in the metal cylinder from the neck down. Air was sucked out of the cylinder by a set of leather bellows powered by a motor; the negative pressure created by the vacuum forced his lungs to expand. When the air was pumped back in, the change in pressure gently deflated his lungs. This was the regular hiss and sigh that kept Paul alive. He could not leave the lung. When medical staff opened it to wash him or manage his bodily functions, he had to hold his breath.
What Paul remembers most vividly about the ward is hearing the doctors talk about him when they walked through on their rounds. “He’s going to die today,” they said. “He shouldn’t be alive.” It made him furious. It made him want to live.
In 1954, when Paul was eight, his mother got a call from a physical therapist who worked with the March of Dimes, a US charity dedicated to eradicating polio. Paul’s months on the polio ward had left him with a fear of doctors and nurses, but his mother reassured him, and so the therapist, Mrs Sullivan, began visiting twice a week.
Paul told the therapist about the times he had been forced by doctors to try to breathe without the lung, how he had turned blue and passed out. He also told her about the time he had gulped and “swallowed” some air, almost like breathing. The technique had a technical name, “glossopharyngeal breathing”. You trap air in your mouth and throat cavity by flattening the tongue and opening the throat, as if you’re saying “ahh” for the doctor. With your mouth closed, the throat muscle pushes the air down past the vocal cords and into the lungs. Paul called it “frog-breathing”.

Sullivan made a deal with her patient. If he could frog-breathe without the iron lung for three minutes, she’d give him a puppy. It took Paul a year to learn to do it, but he got his puppy; he called her Ginger. And though he had to think about every breath, he got better at it. Once he could breathe reliably for long enough, he could get out of the lung for short periods of time, first out on the porch, and then into the yard.
Although he still needed to sleep in the iron lung every night – he couldn’t breathe when he was unconscious – Paul didn’t stop at the yard. At 21, he became the first person to graduate from a Dallas high school without physically attending a class. He got into Southern Methodist University in Dallas, after repeated rejections by the university administration, then into law school at the University of Texas at Austin. For decades, Paul was a lawyer in Dallas and Fort Worth, representing clients in court in a three-piece suit and a modified wheelchair that held his paralysed body upright.
At a time when disabled people were less often seen in public – the Americans With Disabilities Act, which banned discrimination, wouldn’t be passed until 1990 – Paul was visible. Over the course of his life, he has been on planes and to strip clubs, seen the ocean, prayed in church, fallen in love, lived alone and staged a sit-in for disability rights. He is charming, friendly, talkative, quick to anger and quick to make a joke.
At 74, he is once again confined to the lung full-time. Only one other person in the US still uses one. The last person to use an iron lung in the UK died in December 2017, at the age of 75. No one expected someone who needed an iron lung to live this long. And after surviving one deadly epidemic, Paul did not expect to find himself threatened by another.
Poliomyelitis kills by suffocation – not by damaging the lungs, as Covid-19 does, but by attacking motor neurons in the spinal cord, weakening or severing communication between the central nervous system and the muscles. The ensuing paralysis means that the muscles that make it possible to breathe no longer work.
Polio existed in isolated outbreaks around the world for millennia, but it didn’t become epidemic until the 20th century – helped, ironically, by improvements in sanitation. Poliovirus enters the body through the mouth, via food or water, or unwashed hands, contaminated with infected faecal matter. Until the 19th century, almost all children would have come in contact with poliovirus before the age of one, while they still enjoyed protection from maternal antibodies transferred from mother to baby during pregnancy. However, as sanitation improved, children were less likely to come into contact with poliovirus as babies; when they encountered it as older children, their immune systems were unprepared.
In the US, from 1916 onwards, each summer brought an epidemic of polio in some part of the nation. At its peak in the 40s and 50s, the virus was responsible for more than 15,000 cases of paralysis in the US each year. During this same period, it killed or paralysed at least 600,000 people annually worldwide. The year Paul contracted the virus, 1952, saw the largest single outbreak of polio in US history: almost 58,000 cases across the nation. Of those, more than 21,000 people – mostly children – were left with varying degrees of disability, and 3,145 died.

Though polio was not the most lethal of epidemic diseases, it transformed everywhere it touched. “It was like the plague, it drove everybody mad,” Paul told me when I first spoke to him last year. In places where outbreaks occurred, families sheltered in fear at home with the windows shut. All kinds of public gathering places closed. Human interactions were laced with uncertainty. According to the historian David Oshinsky, some people refused to talk on the phone out of concern that the virus could be transmitted down the line. During the first major outbreak in New York in 1916, 72,000 cats and 8,000 dogs were killed in one month after a rumour went around that animals transmitted the disease (they don’t). By the 40s, parents had their children perform “polio tests” every day during the summer – touch their toes, tuck their chin to their chests, checking for pain or weakness – while insurance companies sold “polio insurance” to parents of new babies.
Before the arrival of a vaccine in 1955, what made polio so terrifying was that there was no way of predicting who would walk away from an infection with a headache, and who would never walk again. In most cases, the disease had no discernible effect. Of the 30% or so who showed symptoms, most experienced only minor illness. But a small proportion, 4-5%, exhibited serious symptoms, including extreme muscular pain, high fever and delirium. As the virus hacked its way through the neural tissue of the spinal cord, a few of those infected were paralysed; this progression of the virus was known as paralytic polio. Roughly 5-10% of patients who caught paralytic polio died, although this number was far higher in the days before widespread use of the iron lung.
If we had forgotten the terror of epidemics, we are now being forcibly reminded. The last time I spoke to Paul, in April, it was over Skype, from our respective lockdowns – him in his iron lung in an apartment in Dallas, with a rotating staff of full-time carers and an Amazon Echo next to his head, and me in my house in Surrey, England.
Like polio, Covid-19 can be transmitted by silent carriers who don’t know they have it. Like polio, it has put normal life on hold. And just as with polio, we are pinning our hopes on a vaccine. There is even talk of bringing back the iron lung – a UK-based initiative is trying to bring a new negative-pressure ventilator called Exovent to hospitals for Covid-19 patients. Unlike positive-pressure ventilators, this smaller iron lung would fit over the patient’s chest, allowing them to remain conscious, speak, eat and take medication orally as a machine breathes for them.
“It’s exactly the way it was, it’s almost freaky to me,” Paul said of the parallels between polio and Covid-19. “It scares me.”
Though this virus, if he gets it, will likely kill him, life hasn’t changed dramatically for Paul since the start of the pandemic. He hasn’t been able to venture outside of his lung for more than five minutes in years. As one of his friends told me: “It’s not a strain for him, it’s his life. This is Mr Shelter-in-Place.” I asked Paul if he is worried about Covid-19. “Sure, sure,” he said. Then he added: “Well – I don’t sit around and worry about it. I’m dying a lot. It doesn’t make any difference.”
Paul’s health has always been precarious, but it has declined in the past few years. When I first met him in May 2019, he was a long-term inpatient at Clements Hospital in north Dallas. More than four months earlier, he had developed a persistent respiratory infection, which had sent him to hospital. He also suffers pain in his legs every time he is moved. He had hoped the doctors could help him manage that pain, but, he told me, “It’s not about to go away,” looking up from a pillow on a wide board attached to one end of the lung. His voice is slow, raspy and sometimes punctuated by gasps. Hearing Paul over the machine’s constant sighs requires the listener to focus on him and tune out the lung; accordingly, he is used to being listened to.
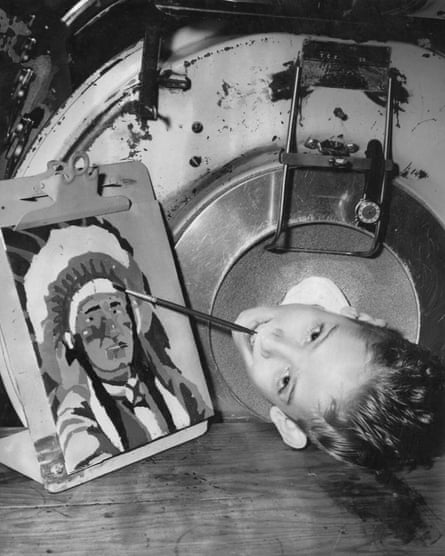
Next to Paul’s head was a clear plastic stick, flat and about a foot long, with a pen attached to the end of it. His father crafted a stick like this when Paul was a child, and he has been using versions of it since. He clamps the end of the stick in his mouth and manipulates the pen to write, type and push buttons on the phone; he used it to sign the hospital’s waiver allowing him to talk to me, although he bristled at having to sign anything at all to tell me his own story. “That is the most ridiculous thing,” he grumbled. Paul’s teeth are flattened and worn from years of using the stick. Though his body inside the lung is scarcely larger than it was when he was a child and his muscles atrophied, his neck measures 18 inches around and his jaw muscles bulge.
Paul’s iron lung – his faithful “old iron horse” as he calls it – is the butter-yellow colour of 50s kitchen appliances. Its metal legs, ending in black rubber wheels, raise it to a height that suits a caregiver, while windows at the top allow them to see inside, and four portholes on the sides let them reach in. To open the machine, which weighs almost 300kg, carers must release the seals at the head and slide the user out on the interior bed. The portholes, the pressure valves, the cylindrical shape and the colour all give the impression of a sturdy miniature submarine.
Iron lungs were built to last, even if no one thought the people in them would. The device was invented in 1928 by Philip Drinker, a medical engineer, and Louis Shaw, a physiologist, at Harvard. Drinker had visited Boston Children’s Hospital to investigate a malfunctioning air conditioner in the ward for premature babies, but he came away haunted what he saw in the polio ward – “the small blue faces, the terrible gasping for air”, as his sister and biographer, Catherine Drinker Bowen, later wrote. His invention was a simple mechanism, doing the job of depleted muscles, and it meant that thousands of children who would have died didn’t. The iron lung was intended to be used for two weeks at most, to give the body a chance to recover.
Over time, the claustrophobic iron lung became emblematic of the devastating effects of polio. Only the sickest patients ended up in one; if they made it out, a lifetime of disability was likely to follow. But once the vaccine was administered to children across the US from 1955, incidence of the disease plummeted. Those who needed short-term breathing assistance were treated by more invasive but much smaller positive-pressure ventilators, invented in 1952 by an anaesthetist during a polio outbreak in Copenhagen. These push air directly into and out of the lungs either through the mouth, via a tube that is snaked down the throat while the patient is sedated, or through a hole made in the trachea. These, like the iron lung, were only intended for short-term use; those few people who needed help breathing for the rest of their lives saw a hole in their throat as an acceptable price to pay for the increased mobility that positive pressure offered. The last iron lungs were manufactured in the late 60s.
By the time positive-pressure ventilators were in widespread use, however, Paul was used to living in his lung, and he had already learned to breathe part of the time without it. He also never wanted a hole in his throat again. So he kept his iron lung.
With the decline of the disease, and the visual reminders of it hidden away in a handful of homes and care facilities, across much of the western world the terror of polio faded from collective memory. “You can’t believe how many people walked into my law office,” Paul said, “and saw my iron lung and said: ‘What is that?’ And I’d tell them: ‘It’s an iron lung.’ ‘What does it do?’ ‘Breathe for me.’ ‘Why?’ ‘I got polio when I was little.’ ‘What’s polio?’ Uh oh.” David Oshinsky, the author of Polio: An American Story, believes that the success of vaccines in eradicating so many deadly diseases is precisely why the anti-vaxx movement has gained ground in recent years. “These vaccines have done away with the evidence of how frightening these diseases were,” he told me.
When I visited him at Clements Hospital, Paul seemed like a kind of medical celebrity – none of the hospital staff had ever seen an iron lung before. As we talked, two women in nurses’ scrubs came in. They were from another unit, but they just wanted to meet the man in the iron lung, they said. Paul told them that he was in the middle of an interview. “That’s all right, sir,” the older nurse said, “we’ll just listen for a bit.” After they left, Paul told me this happens all the time. “That’s the way it is – like living in a zoo,” he said.
People often come away from meeting Paul humbled. Norman Brown, a retired nurse who has been good friends with Paul since 1971, said: “The guy is such an impressive character … most people are in awe when they first meet him.” Paul doesn’t mind answering people’s questions: “I’m a lawyer, I’m paid to talk!” He likes talking about polio and the lung, and about his life, because what terrifies him, even more than the possibility of Covid-19, is that the world will forget what polio was like, and what he achieved in spite of it.
On Christmas Eve 1953, a year and a half after Paul was admitted to Parkland Hospital, his parents rented a portable generator and a truck to bring him and his iron lung home. It was a short, nerve-racking drive: “Any minute it looked like that old generator would go off,” his father Gus later told a Texas newspaper. “It kept popping. I didn’t know if we would make it home or not.” Part of the reason Paul was cleared to leave the hospital was that no one expected him to live much longer.
But Paul didn’t die. He gained weight; the day he got home, his older brother made him a plate of bacon – the best he’d ever tasted, he said. His parents slept in the same ground-floor living room with him, always half-awake in case the swish-swish of the machine stopped. It did during power cuts – even today, Texan storms and tornadoes sometimes knock down power lines – and his parents had to pump the machine by hand, calling neighbours in to help.
After three years, Paul could leave his lung for a few hours at a time. His frog-breathing had become muscle memory – like riding a bicycle, he told me. His education had been left to founder during his 18 months on the ward. One day, his mother walked in with a pile of books borrowed from the local elementary school: she was going to teach him to read.

“I had all these ambitions. I was going to be president,” he said. But it took his parents, along with the parents of several other disabled children, more than a year to convince the Dallas school system to allow him to take classes from home. In 1959, when he was 13, Paul was one of the first students to enrol in the district’s new programme for children at home. “I knew if I was going to do anything with my life, it was going to have to be a mental thing. I wasn’t going to be a basketball player,” he told me.
Most days, he would leave the lung around the time other children got out of school, and sit out front in his wheelchair. Friends would push him around the streets; later, as they got older, the same friends took him to diners and cinemas, then restaurants and bars.
And he went to church. The Pentecostal church, to which the Alexanders belong, is a denomination characterised by a personal, passionate experience of God. At the end of each service, congregants are invited to come to the front of the church and pray. “My dad would take me down there sometimes to pray with him, and he would let all of his emotions out then,” Paul’s younger brother, Phil, told me. “He’d just cry and cry.”
Paul dealt with his emotions in a different way. Polio had robbed him of his independence. “He let his anger out a lot. He had a mouth,” Phil recalled. “I completely understand it. He would yell and scream and curse and get it all out, and my parents would just let it happen, because obviously, Paul would need a release … he was normal.” It hurts Paul to think about it now. “There were frustrating times, times I’d get really mad, scream. But Mom and Dad were so tolerant, they seemed to just understand,” he said. As he spoke, tears trickled down his temple to the pillow.
In 1967, Paul, now 21, graduated from high school with almost straight As. His one B was in biology, because he was unable to dissect a rat. “I was so mad,” he said. (He still is.) He applied to Southern Methodist University in Dallas, but despite his academic record, he was rejected. “I was too crippled,” he said bitterly. “Broke my heart. I fought for two years, repeatedly called them. “‘Well, wait a minute,’ I’d say, ‘I want you to reconsider, think about this. I’m coming over, I want to talk to you!’” His high school teachers backed him. Eventually, the dean of admissions relented, on two conditions: that he find someone to help him get to his classes, and that he get the polio vaccine.

Paul was “scared to death” rolling into his first class. “You have to understand, back then, there were no cripples. There was none on campus, I was the only one. Wherever I went, I was the only one. Restaurant, movie theatre – I thought: ‘Wow, there’s nobody else out here. I’ll just pave the way,’” he said. “I kind of thought of myself as representing a group. I fought for that reason. ‘What do you mean I can’t go back there? I want to go back there!’ … ‘You can’t do that.’ ‘Oh yes I can!’ I was always fighting.”
Paul met a woman, Claire, and fell in love. They got engaged. But one day when he called, her mother – who had long objected to the relationship – answered, refused to let him talk to her, and told him never to speak to her daughter again. “Took years to heal from that,” he said. He transferred to the University of Texas at Austin. At Southern Methodist University, he’d been living at home, but now he was on his own. His parents were terrified.
At UT, the caregiver Paul had hired never turned up, so for a month, the guys in his dorm took care of him – even “the most intimate things”, he said – until he was able to hire a new one. Paul graduated in 1978, and later began studying for a postgraduate degree in law. He again made headlines in November 1980: “Iron-willed man leaves iron lung to vote”, declared an article in the Austin American Statesman newspaper.
Paul struggled with trying to pay for a full-time carer and his education at the same time, but in 1984, he graduated from the University of Austin with a degree in law, and found a job teaching legal terminology to court stenographers at an Austin trade school. When a newspaper reporter asked if his students found it uncomfortable to be in his class, he responded: “I don’t allow people to feel uncomfortable for very long.”
He passed his bar exams, and on 19 May 1986, he slightly raised his right thumb as he took the oath promising to conduct himself with integrity as a lawyer in front of the chief justice of the supreme court of Texas. He was 40 years old, wearing a natty three-piece suit, living on his own, and able to spend most of his day outside the machine that still kept him alive.
The story of how Paul taught himself to breathe is central to how he thinks about himself. It represents the determination that made everything else – getting into university, the law degree, the life of relative independence – possible. It even inspired the title of the memoir, Three Minutes for a Dog, that he self-published in April. It took him more than eight years to write it, using the plastic stick and a pen to tap out his story on the keyboard, or dictating the words to his friend, former nurse Norman Brown.
But the title of the book was Kathy Gaines’s idea. Kathy, 62, has been Alexander’s caregiver since he graduated from law school and moved to the Dallas-Fort Worth area, although neither can remember precisely when she found his advert in the paper and became his “arms and legs”.
Kathy is a type-1 diabetic and, as a consequence of the disease, has been legally blind for years, so she can’t drive. During Paul’s five-month stay in hospital last year, she took the bus or got a lift there every day. She taught the nursing staff how to manage the machine and, to some degree, Paul. While we talked, Kathy brought us foam cups of hospital coffee, and a plastic bendy straw for Paul. She left it close enough for him to reach with his tongue and mouth, but not so close as to be in the way. Kathy knows how to shave Paul’s face, change his clothes and sheets, trim his hair and his nails, hand him his toothbrush, do his paperwork, make his appointments, do his grocery shopping, and that when he says “biscuit” he usually means “English muffin”. Sometimes, if she sees his head in a position that she thinks will be uncomfortable for him, she’ll move it without asking. (He doesn’t always appreciate that.)
Kathy knows everything about him, Paul says. “Kathy and I grew together … she stretched herself over as many things as I needed,” he said. For most of their relationship, Kathy has either lived with Paul or nearly next door. They’ve moved a lot: his legal career was not lucrative, and he has struggled financially. Today, Kathy lives upstairs in their communal apartment building. She sees him every day, whether she’s working or not.
Though Kathy and Paul have never been romantically involved, his brother Phil describes their relationship like a marriage. “Paul has always been aggressive about things that he wants and needs around other people,” he said. “He’s pretty demanding. But Kathy is more demanding than he is. They’ve had their moments, but they always work it out.”
Paul has always craved independence. But his life depends on his caregivers showing up for work, on his iron lung not blowing a gasket, on the electricity staying on. “He’s been 100% depending on the kindness of others since he was six years old – 100%. And he’s done it by virtue of his voice and his demeanour and his ability to communicate,” said Norman Brown. “I would do things for him that I wouldn’t do for people. For example, he got evicted from an apartment, and he says: ‘I want to egg that manager’s door.’ And when he says ‘I want to do something’, he means you’re going to do it. So we got a bunch of eggs and drove over to that manager’s apartment,” Brown said, laughing.
What Paul hates is being invisible. He remembers going to restaurants where the server asked his companion, “What will he be having?” His voice shook with anger at the memory. “I think it’s why I fight so hard, because there’s people standing there with the gall to tell me what I’m going to do with my life … You have no right to tell me what to do,” he said. “You should get down on your knees and thank God it wasn’t you.”
Paul has now outlived both his parents and his older brother, Nick. He has outlived his old friends. He has even outlived his original iron lung. In 2015, the seals were failing and it was leaking air. Not surprisingly, spare parts for iron lungs, and mechanics who know what they’re looking at, are difficult to find, but after a friend posted a video of Paul on YouTube asking for help, a local Dallas engineer fixed him up with a refurbished one.
Paul still has big plans – he has hopes that his memoir is “going to smack across the world” – but Covid-19 is a new danger. Paul is, Phil said, “probably the most vulnerable you can get” to a virus like this one. “He’s staying positive, but we’ve also had conversations that this is probably going to do it. It’s very likely.”
Paul has always thought that polio, the “demon” that tried to destroy him, was going to come back. “I can see hospitals inundated by polio victims again, an epidemic, I can see it so easily. I tell the doctors, it’s going to happen. They don’t believe me,” he told me when he was in hospital last year.
It is only thanks to concerted vaccination efforts that there hasn’t been a new case of polio in the US since 1979, or in the UK since 1984. By 2000, the World Health Organization had declared all of the Americas and the western Pacific region polio-free. India, which had seen 200,000 cases of polio a year through the 1990s, was declared polio-free in 2014 after a series of aggressive vaccination campaigns. The virus is now only endemic to three countries in the world – Afghanistan, Nigeria and Pakistan – and cases of polio number in the dozens.
